(Source): Quartz: https://qz.com/1429001/the-opioid-epidemic-is-tearing-communities-apart-heres-how-one-city-came-together-to-fight-it/
The opioid epidemic is tearing communities apart. Here’s how one city came together to fight it
 Emma is rocking her baby, speaking to her softly in the neonatal intensive care unit of Winchester Medical Center in the city of Winchester, Virginia. The blinds are drawn and the room is quiet. A cheerful poster on the wall says that Emma’s daughter, Story, was born six days ago. She weighs six pounds and 13 ounces.
Emma is rocking her baby, speaking to her softly in the neonatal intensive care unit of Winchester Medical Center in the city of Winchester, Virginia. The blinds are drawn and the room is quiet. A cheerful poster on the wall says that Emma’s daughter, Story, was born six days ago. She weighs six pounds and 13 ounces.
But Story isn’t like most other newborns. In her first days of life, she is going through withdrawal from the opioids that her mother took while she was pregnant, leading to a condition known as neonatal abstinence syndrome, or NAS.
In the US, NAS rates are on the rise. The best estimates suggest that in 2012, 21,732 babies were born with the diagnosis, meaning that one baby was born with NAS every 25 minutes—and many doctors say that’s probably an underestimated figure. Babies born with NAS suffer from short-term health problems for up to six months after birth (including diarrhea, vomiting, high fevers, and seizures), as well as potential long-term behavior, developmental, and health consequences, many of which are still unknown as scientists grapple with the unanswered questions of the long-term outcomes for infants exposed to opioids.
The large majority of NAS babies are covered by Medicaid (pdf), but the disease is expensive to treat. Accurate national estimates are hard to come by because every state, and sometimes every hospital, has a different way of reporting NAS. At Winchester, however, the average cost of treatment for NAS is more than $47,000 per infant (pdf)—though, as the Winchester city council has stated, “the costs to the community in terms of actual expenditures, resources and human life caused by substance abuse and addiction are extraordinarily significant, if not incalculable.”
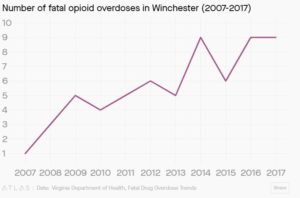
Winchester is a small city of less than 28,000 people that has suffered from the opioid epidemic ravaging the United States—a public health crisis so large that it takes the life of about 115 Americans every single day. In Virginia, fatal drug overdoses are the leading cause(pdf) of unnatural death, and have been since 2013. In Winchester and its five surrounding counties, opioids killed 40 people last year; as of June 2018, they had already killed 13 people.
And yet Winchester’s story is not a tragedy, because even as the city grapples with addiction, it has earned a reputation for having created a uniquely strong community-led response to the opioid epidemic. What accounts for its impact? The answer, it turns out, comes down to the vision of its community leaders—including dedicated doctors and nurses, a tireless public defender, a determined chief of police, a few frustrated judges, and an addict-turned-pastor devoted to helping his community recover. What they have accomplished represents a possible blueprint for addressing the opioid crisis, one that has less to do with law enforcement and more to do with community and compassion.
The babies of the opioid epidemic
 Emma, whose name has been changed to protect her privacy, is 28 years old. From the way she adjusts Story’s blanket so she doesn’t get cold, or sways her back and forth to soothe her when she cries, it’s clear she loves her baby. Cradling Story in her arms, she begins her tale: How she went from being a well-adjusted high school graduate to an addict sustaining her habit by working as an exotic dancer.
Emma, whose name has been changed to protect her privacy, is 28 years old. From the way she adjusts Story’s blanket so she doesn’t get cold, or sways her back and forth to soothe her when she cries, it’s clear she loves her baby. Cradling Story in her arms, she begins her tale: How she went from being a well-adjusted high school graduate to an addict sustaining her habit by working as an exotic dancer.
She was 20 years old and working as a private special-needs tutor when she began dating a boy she’d gone to high school with. Within a few months, they married. “I had spring fever, badly, but it was a complete joke,” Emma says, looking sad.
Her husband was a heroin addict, and they started transporting heroin across state lines, to and from Baltimore, on what’s known as “heroin highway”—the corridor along Interstates 70 and 81 that begins in Baltimore and runs through Maryland, West Virginia, and Virginia. They hoped to make money. Instead, they ended up using a lot, and making very little.
Six days into their marriage, Emma’s husband went to jail. He stayed there for a year, then was released, but was sent back for breaking the terms of his probation. During his second stint in prison, Emma served him with divorce papers. Meanwhile, for the first time, Emma was exposed to Dilaudid, a powerful opioid made from morphine and used for pain management. She got hooked, and became an exotic dancer to sustain her habit.
Emma was in and out of treatment for many years, but nothing stuck. One day, grieving over the death of another close friend from an overdose, Emma mixed two different types of drugs and overdosed herself. Emergency responders revived her with naloxone, a medication used to block the effects of opioids. The experience clearly marked her: “It was one of the strangest things I’ve ever experienced,” she says. “I was, like, dead. Dead. It was so weird. Because I remember what I saw.”
Her near-death experience convinced her to go into methadone treatment, an opioid that helps addicts taper their dependence. She admits, though, that she only stopped taking heroin; she was still doing cocaine and taking benzodiazepines. In the world of drug addiction, “clean” is in the eye of the beholder.
Two months into her treatment, Emma found out that she was pregnant by her boyfriend, Nick. (Nick’s name has also been changed.) According to Emma, this was an accident—albeit a happy one. “I never thought I could have kids, ever, so she was a surprise,” she says. “And I’ve always wanted kids.” She stopped taking drugs, except for her methadone treatment, which she stayed on because she knew that, if she quit, she’d be back on opioids and heroin the next day.
But babies in the womb don’t discriminate between prescription drugs and street drugs, or between opioids taken as part of a treatment plan and opioids taken because of an addiction. Any fetus exposed to opiates, like morphine, fentanyl, or methadone, or even other substances like antidepressants or benzodiazepines, has a high chance of developing NAS. And, while not every baby with NAS needs medically-assisted treatment—for some, a few days in a nurturing environment after birth is enough to rid them of their symptoms—anywhere between 55% and 94% of substance-exposed infants develop NAS symptoms, depending on the severity and regularity of the drug exposure, and the additional lifestyle risk factors, like the number of drugs they used simultaneously, or heavy alcohol use.
Emma’s decision to stay on methadone during her pregnancy, knowing that it would increase her daughter’s chances of being born with NAS, was a complicated one. “My family was pressuring me, and my boyfriend was pressuring me to come off it,” she explains, but hearing from her doctors convinced her she should stay on her treatment plan. “The methadone saved my life,” she says. “I know myself well enough to know when I’m ready, when I’m not, and what I do when I come off of it if I’m not ready: I go back [to drugs] every time. So, I’m safe where I’m at,” she adds. She says her pregnancy, and becoming a mom, has taught her a lot about herself. “In a lot of ways, I’m really thankful for the whole experience. I wish that my baby wasn’t exposed, but I’m glad that she wasn’t exposed to worse.”
What does withdrawal look like?
Watching a baby go through opioid withdrawal is heartbreaking. The symptoms can include high-pitched, inconsolable screaming, shaking, difficulty keeping any food down, fevers, vomiting or diarrhea, and stiff limbs, which leads to sudden jerking movements.
To wean babies off the drugs which they’ve become unwittingly dependent on, doctors typically use one of two possible treatments: either methadone, the same opiate used to treat adult drug addicts, or a combination of morphine and clonidine. The combination of morphine and clonidine has to be given out in regular doses over a longer period of time than the methadone, meaning that babies have to stay longer in the NICU. But the doctors at Winchester think it’s ultimately better than methadone, which requires frequent doctor’s office visits after discharge and prolongs the baby’s postnatal exposure to opiates.
So, at Winchester, babies with NAS get morphine and clonidine; but even the doctors there are unsure about what the long-term impact of the treatment may be as the babies grow up. That’s because very little is known about the long-term effects of either treatment. “There are no studies in the literature of the long-term developmental outcome of babies who went through NAS,” says Barry Lester, a developmental psychologist at Brown University who was the principal investigator of the Maternal Lifestyle Study, a 16-year landmark longitudinal study of babies exposed to cocaine in utero. Lester and his colleague, Jonathan Davis, are conducting the first national clinical trial to measure the difference in long-term development between substance-exposed babies treated with methadone or morphine. The two experts recently finished an 18-month follow-up with these infants, but the results are not yet available. And in the meantime, hospitals will continue to make their best guesses about appropriate ways to care for NAS babies.
The nurses at Winchester say they are often asked about how a mother could do this to her child. It’s a fact of this drug crisis, as well as past ones, that mothers with addiction are often disproportionately judged for putting not only themselves at risk, but also their babies. Despite the fact that doctors have developed a greater understanding of the biology of addiction, mainstream attitudes haven’t caught up. Addiction hijacks the brain’s neurotransmitters to bind someone to the high of their drug of choice. Science tells us that addicted moms go through biological changes in oxytocin and dopamine production in the brain—the neurotransmitters involved in regulating movement, emotion, motivation, pleasure and reward. An addict’s drug use overwhelms the feelings triggered by naturally rewarding behavior—like caring for a baby—and becomes the primary motivator in that person’s life, governing the choices a female addict might make during pregnancy.
The moral panic surrounding women’s opioid use during pregnancy has a historical precedent in the reactions to the widespread use of crack cocaine in the late 1980s and early 1990s in the US, when the medical community and the general public wildly overstated the negative effects of cocaine on children. But Lester, who studied the “crack baby” hysteria, says that we don’t yet have enough information to fully understand the long-term impact that NAS will have on these children. As he told The New York Times, “You have to realize that there is a certain amount of prejudice against women who use drugs. The expectation—almost the wish—is that there’ll be something wrong with these kids so we can blame these mothers again, like we love to do.”
Winchester and the opioid crisis
Communities like Winchester aren’t unique. Across the US, there are millions of them: It’s a small, majority-white town that used to be home to large manufacturing plants, which closed down in the 1980s, putting hundreds of people out of work.
And it has a drug problem (pdf):
Moms who have taken drugs during pregnancies, or parents of babies born with NAS, are referred to one of these services, depending on the gravity of their situation. In 2017, Winchester referred 191 substance-exposed newborns to these services; as of June 19th, 2018, they had referred 92.
These numbers might not sound huge, but Winchester is just one small city in one locality of Virginia. State-wide, the total number of NAS hospitalizations increased from 741 in 2016 to 819 in 2017, an 11% increase in one year. Nationally, the numbers are staggering(pdf): Rates of NAS increased by 300% between 1999 and 2013 (though not all of these cases resulted in hospitalization).
Because babies who have been exposed to drugs are treated in hospitals, which are mandated to report their condition to state authorities or to volunteer family services, these places are one of the best markers we have for the evolution of the opioid epidemic, and its impact on a generation of children. That’s why the Winchester NICU was first to understand the growing crisis affecting the community; and the first to do something about it.
The power of community
Winchester’s approach to tackling the opioid epidemic isn’t revolutionary, but it is uniquely effective. It is characterized by an unusually active local coalition of actors impacted by substance abuse and addiction in the Winchester region, called the Northern Shenandoah Valley Substance Abuse Coalition, a progressive law enforcement effort, and the contributions of the local community, from religious leaders to neighborhood volunteer groups.
When Daniel Carey, Virginia’s secretary of health and human resources, came into office, he asked where the high-performing communities tackling this crisis were. Winchester and the Northern Shenandoah Valley were at the top of the list. “What stands out about Winchester,” he explained, are “some of the commitments they’ve made,” including “a very strong local coalition” and the uniquely close relationship between the Community Services Board (CSB) and the Winchester Medical Center. That relationship allows for what Maria Delalla describes as a “continuum of care for substance-exposed newborns” after their discharge from the hospital. It has led to innovative forms of treatment, including when CSB had the idea to embed a mental health counselor within the obstetrics offices at Winchester to work with substance-dependent pregnant women. That’s important because qualified health professionals meet with women as early as possible in their pregnancy to create what they call a “plan of care” for each woman that includes individualized short- and long-term planning for their child’s education and treatment.
Jay Bhatt, the senior vice president and chief medical officer of the American Hospital Association (AHA), says that, during the time he has been at the AHA, he has both heard about and learned from the work that Winchester has been doing. “They found a way and a systematic approach for a dynamic, multi-disciplinary [strategy],” he told Quartz. “We have law enforcement, public health, health systems, child welfare, family courts, county and city leadership, and community members that are affected by the crisis. The ability to bring those partners together is not easy, and to do that for this purpose is one of the things that, to me, is very interesting about Winchester’s approach.”
For Teresa Clawson, one of the neonatologists of the Winchester NICU, the crisis started in 2009. That’s when she first noticed an uptick in the number of babies being diagnosed with NAS.
The opioid epidemic was already in full swing by that point, when the United States consumed 99% of the world’s hydrocodone, 60% of the world’s hydromorphone, and 81% of the world’s oxycodone. Local, state, and federal authorities were slower to catch on to the magnitude of the crisis. That’s no longer the case, but it’s arguably too late. In 2017, president Donald Trump declared the opioid crisis a public health emergency. Changes in prescription practices, driven by the Department of Health and Human Services and rising public awareness of the problem, have finally reversed trends in opioid prescriptions. Even so, in 2017, there were almost 58 opioid prescriptions written for every 100 Americans.
To Clawson and her team, it was obvious early on that there was a problem. She formed the Perinatal Substance Abuse Task Force, a multidisciplinary group of health care providers, social services/child protective services, early intervention specialists, mental health counselors, and drug treatment providers. The task force started training medical staff on the science of addiction, implementing universal urine drug testing of all expectant moms at Winchester, and even lobbying the Virginia State House to give doctors more time to report cases of NAS to state authorities after toxicology tests.
Meanwhile, in September 2013, the public defender for Winchester and its surrounding counties, Timothy Coyne, went to a Redskins game with Nicolas Restrepo, the vice president of medical affairs for Winchester Medical Center. They got to talking about how their work was going. Each of them was dealing with the disproportionate rise of deaths and overdoses from heroin in the community in their own ways. For Restrepo, it meant an increase in violent incidents in the ER at Winchester; for Coyne, it meant a higher number of clients “who were dying, overdosing, even while their cases were pending.”
Coyne and other members of the law enforcement community began pushing hard to set up a better legal system to prosecute drug users in Winchester, because, as Coyne explains, “we cannot arrest our way out of this problem.” In the meantime, the staff of Winchester Medical Center were setting up protocols for opioid prescriptions, training medical staff in addiction resources and the treatment of NAS, and launching an extensive community outreach program.
But residents of Winchester say things really began to change with the advent of the region’s first drug court, which was brought about by two major local summits on the drug crisis.
When people recall those summits, they usually tell the same story: Then-chief of police Kevin Senzenbarcher addressed the room and said that the community couldn’t arrest its way out of the drug epidemic. He invited anyone interested in finding a solution to hand him their business card.
Coyne and Restrepo were among those who stepped up to help. They co-led a committee on “best practices” to learn from other areas of the country and see what worked and what didn’t. One major idea that came out of those conversations was a drug court.
Drug court programs are unique because they’re designed as an alternative to processing drug users through the normal court system, with the goal of reducing drug use and encouraging defendants toward recovery, not prison. They’re usually run by a team of judges, prosecutors, addiction and treatment specialists, and defense attorneys. They’ve been shown to lower recidivism, lower the costs of drug treatment, and encourage addicts to complete drug treatment. They’re also increasingly common in the US: According to the National Institute of Justice, there were more than 3,100 drug courts as of June 2015. And support for drug courts also appears to be growing: During the 2017 fiscal year, over $100 million in federal funding (pdf) was appropriated to states and localities to support the creation and enhancement of drug courts.
Coyne lobbied county administrators, city council, and city administrators to set up a drug court in Frederick county, where Winchester is located. In 2016, he got his wish.
The Northwestern Regional Adult Drug Treatment Court was established in August 2016, with the help of juvenile court judge Elizabeth Kellas. So far, the drug court has served 38 clients, all of them non-violent offenders. Four people have fully graduated from the program, with another one expected to graduate this month. Two years in, according to Coyne, it’s already made a difference in the community: “The drug court is creating an alternative to incarceration for a lot of our folks that are charged with non-violent crimes,” he said.
Since only a few people have completed the 12-16 month drug program so far, Coyne doesn’t have much data on its impact in terms of recidivism. But anecdotally, he says his clients are “totally different people, even three or four months into the program.”
Judges and federal prosecutors around the US have echoed that sentiment. According to a brief prepared by the Superior Court of California, “Unequivocally, judges involved with drug court programs maintain that the drug court approach is much more effective than the traditional criminal case process for the significant number of offenders who seriously desire to address their substance addiction and turn their lives around.” The same goes for prosecutors and police, who report that the drug court in their jurisdictions “significantly enhances the credibility of the law enforcement function, provides their agencies with a more effective response to substance abuse, and is a significant alternative to the ‘revolving door’ syndrome that has frequently resulted from the traditional case process.”
It’s hard to tell yet whether these community programs, like the drug court or the NSVSAC, have had any measurable impact on the number of people dying of substance abuse in Winchester and the surrounding counties. But hospital officials say they have seen a change: Now that all mothers are screened for drug use, the hospital has gotten much better at identifying babies with NAS. The NICU has also gotten better at treating babies born with addiction.
Before Clawson and the team in the NICU put in place their NAS treatment protocol, the average length of stay in the NICU of a substance-exposed infant was 54 days. Now, it’s down to 22 days. That means less hospital time for babies and parents, as well as less drugs being pumped into babies’ systems. Before the protocol was put in place, NAS babies were on morphine for an average of 30 days, and on clonidine for an average of 44 days. Now, they take morphine for an average 18 days, and clonidine for 20 days.
Clawson says the credit for these results go to the NICU’s neonatal abstinence syndrome committee: “This is the result of caring more than others think is wise for addicted parents who have historically been cast aside; risking more than others think is necessary to encourage parents with the disease of drug addiction to be active participants in their babies’ care; and expecting more than others think is possible, to believe in each other and as a team to confront this difficult professional situation, and to believe in the families that we serve.”
The many faces of compassion
Several other major initiatives came out of the 2014 summits. That summer, Valley Health began training emergency departments and urgent care centers in how to properly prescribe opioids and educate patients about the risks of addiction. Also in July 2014, the medical center partnered with Casey Family Programs and launched an extensive community outreach program (pdf), which included putting out ads in local magazines (pdf), organizing health and safety fairs to educate the community about drug addiction, and funding peer-to-peer recovery coach training. Jay Bhatt of the AHA described these initiatives as some of the highlights of Winchester’s response. And in January of 2015 the Northern Shenandoah Valley Substance Abuse Coalition was born. The group organizes events to raise awareness about substance use and addiction, including concerts, rallies, coffee chats, and support groups, and collaborates on drug prevention initiatives with community partners, like sheriff’s office or the hospital.
“We have a lot of compassionate individuals in our community,” says Lauren Cummings, the executive director of the Northern Shenandoah Valley Substance Abuse Coalition (NSVSAC). “So many people were realizing that this epidemic did not discriminate,” she added. But changing hearts and minds—given the stigma surrounding drug use and especially around drug-addicted mothers—wasn’t easy. That’s why “one of the first things we did was put a face on this epidemic,” Cummings said.
 That face was Brad Hill, a pastor and recovering drug addict who moved to Winchester in 2012. Hill started a congregation of recovering addicts in 2014, in the back of a bar in downtown Winchester called Brewbakers. The congregation was named Grace Downtown of Winchester—but Hill says the locals call them the “Church of the Addicts.”
That face was Brad Hill, a pastor and recovering drug addict who moved to Winchester in 2012. Hill started a congregation of recovering addicts in 2014, in the back of a bar in downtown Winchester called Brewbakers. The congregation was named Grace Downtown of Winchester—but Hill says the locals call them the “Church of the Addicts.”
Eventually, the group got so large that they had to find a space of their own. On April 1st, 2018, during Easter, Hill’s congregation opened its doors in a more formal church building—and 425 people attended the first service. The church’s mission is explicitly to help people going through recovery or addiction. It hosts narcotics anonymous meetings, organizes “new believers” classes geared towards women struggling with addiction, and run weekly peer-to-peer sessions with community specialists. Hill says that nobody asks to be an addict; he certainly didn’t. “I believe that addiction is not a moral failing,” he says. “Not only am I a pastor, but I’m an addict trying to stay clean.”
An army of cuddlers
Another key initiative came about in 2015. That’s when Winchester began recruiting its first crop of volunteer cuddlers—community members who would come into the NICU once or twice a week in two-to-three hour shifts to hold babies, especially those with NAS, in their arms.
That’s because the best treatment for any child going through NAS is skin-to-skin contact with a caregiver, which supports early breastfeeding and helps regulate babies’ temperature. Emma has clearly been told this one too many times; “mom, family, skin-to-skin contact, someone being there and loving her, that’s what helps her,” she repeats over and over again.
But for a variety of reasons, the parents of babies born with NAS aren’t always able to be with them. That’s when volunteer cuddlers come in. Most of the volunteers are retired and have families living out of state. As one cuddler said, “I get my baby fix that way.” Demand is so high that there’s a wait list for the program, and volunteers can “gift” shifts to friends who want to participate.
Winchester resident John Myers, one of Winchester’s first volunteer cuddlers, has a daughter in Oregon and a son in Massachusetts. His only grandchild lives in Oregon, and he Skypes with her weekly—but, as he explains, it’s not the same thing as holding her in his arms.
The NICU staff speaks very highly of John, and they call him “the baby whisperer.” He’s very tall, endearing yet reserved, and he’s the only cuddler who can hold twins in both arms at the same time—a fact he seems very proud of. He’s even more proud of the fact that he was the first volunteer to ever receive a Friends of Nursing Award, a testament, the nurses explain, to how invaluable he is to helping these babies.
But there’s an undercurrent of anxiety that accompanies his volunteer work as well. “I’ve gotten attached to quite a few babies,” John said. “And the toughest part for me is to say, ‘after you’re not here anymore, what’s your life going to be like?’ You hope for the best but you don’t get any follow-up, and then you move on to the next one.”
He, like most of the cuddlers, deal mostly with babies with NAS, who are often inconsolable and difficult to take care of. “I think sometimes you actually see agony, and that’s really hard,” John explains. “It’s a tough way to start your life.”
Other community members have stepped up, too. The local Rotary Club has provided funding for taxi vouchers and housing subsidies for people coming out of the drug court treatment program, and have helped the NSVSAC apply for grants. Lauren Cummings and her staff put out an ad in the local paper last year asking for donations of professional attire for the people coming out of drug court-mandated treatment. She says her office was overwhelmed with the response: “Our community’s willingness to embrace the drug treatment court says something about their willingness to help people.”
The opioid epidemic has ravaged small communities across the United States. But Winchester seems to have created a system that pushes treatment over incarceration, and support over judgement—or, as Coyne tells it, “Not just government stepping in and … throwing money at the problem.”
Carey agrees that’s a major step in any community’s response: “If you can get communities to treat it as a public health problem, as opposed to a moral failing, then you’ve made a big improvement, and you’ve opened up a different set of solutions.”
 Emma’s baby daughter, Story, is arguably better off than most of the babies that go through the Winchester NICU, and thousands of similar NICUs across the United State. She has a mother who is now clean and cares deeply for her, as well as access to quality medical care. She’s the exception, not the rule: On one spring day in Winchester, four of the 30 babies in the NICU are going through withdrawal, and Story is the only baby whose parent is with her. Two of the babies’ moms are in jail, and another is prevented from seeing her baby by child-protective services. There are also absentee parents—those who never show up to their appointments, or who leave their babies with other family members and continue to take drugs.
Emma’s baby daughter, Story, is arguably better off than most of the babies that go through the Winchester NICU, and thousands of similar NICUs across the United State. She has a mother who is now clean and cares deeply for her, as well as access to quality medical care. She’s the exception, not the rule: On one spring day in Winchester, four of the 30 babies in the NICU are going through withdrawal, and Story is the only baby whose parent is with her. Two of the babies’ moms are in jail, and another is prevented from seeing her baby by child-protective services. There are also absentee parents—those who never show up to their appointments, or who leave their babies with other family members and continue to take drugs.
Clawson says she feels for those parents: “Mothers love their babies. Parents love their babies. And they often feel terribly guilty for what their baby is going through, and sometimes they react to that by not being present, because that’s so difficult to see.”
Because babies with NAS are the innocent bystanders of this public health crisis, they’ve often attracted people’s empathy and pity, much more so than the mothers who are blamed for their condition. Fundamentally, that’s because humans are inclined to see babies as a chance at redemption. As Clawson explained, “I see a baby as someone who might some day contribute something good to this world, and … who will make it a better place than it was before he or she existed.”
That’s why the people of Winchester fight so hard, she says; the babies represent their collective faith in the future. “The ultimate expression of hope is worth fighting for,” she said at a rally in 2016. “I guess you could say I am addicted to hope.”
If you or someone you know is struggling with addiction, please call 1-800-662-HELP (4357).
Read more from our series on Rewiring Childhood. This reporting is part of a series supported by a grant from the Bernard van Leer Foundation. The author’s views are not necessarily those of the Bernard van Leer Foundation.
Correction: An earlier version of this article misstated the reason why doctors at Winchester prefer to treat NAS babies with morphine and clonidine, rather than methadone. Morphine and clonidine treatment requires frequent dosing that would preclude home use.